chiropractic
Visualization and Mental Practice- Take Off Your Shirt and Charge Around Like You Are On Fire. The Wold Cup Goal Will Be Soon To Follow.
My first experience with mental training came in the second grade. I was at recess playing my first game of rugby. We were uncertain of the rules and it took me only 10 minutes to find a way to break my collar bone. Clavicle fractures are common and pretty painful. Where the x-rayed clavicle once held smooth margins it was formed into the shape of a jagged X. I wore a butterfly brace and initially a sling too. After a couple of weeks, the orthopedist called my parents to schedule a time for me to come into the office and begin moving the arm again. My parents were delighted to tell him that I wasn’t available because I was on the mound pitching for my little league baseball team.
My parents love that story. They take full credit for my rapid healing due to the fact that they had me practice a healing visualization each night as I went to sleep. As I remember it I pictured a video game similar to Centipede where I blasted bits of material into the cracked bone.
 |
| An example of an effective visualization for manifesting butterflies. |
The world is full of successful people who have built empires or defeated diseases who will tell you that positive visualization was pivotal to their success. If you think the guy in the picture above got where he is today without some solid mental practice think again. Bill Starr recently published an article detailing the techniques he successfully implemented in competitive olympic lifting for decades. Now that he has retired he continues to use these same visualization techniques every night to prepare for for running errands the next morning. That may appear a little OCD for most people who would rather being doing instead of visualizing but does it really work, and if it does why?
The overwhelming majority of research on the topic of mental imagery/ mental practice is supportive and is statistically relevant. From healing times in stroke victims,(1,2,3) burn victims, (4) depressives (5) to performance based outcome measures,(6,7,8) mental practice has been well studied and its utility validated.
Based on these studies and many others we could say that Mental Practice “works,” but research is never very good at explaining why something works. For that, you have to turn away from the measurables of research labs and into the touchy feely world of metaphysics and philosophy.
Visualization is a skill that improves with practice. There are many different approaches and step by step models to follow that all basically revolve around visualizing yourself accomplishing a task with as much detail as is possible without getting distracted during the process. Techniques involve engaging as many of your senses as possible to effectively create the scenario and engage your nervous system.
It was proposed by Geshe Michael Roache in The Diamond Cutter and in popular New Age films such as What the Bleep Do We Know, and The Secret that any technique can work but only if it effectively convinces some part of your conscious or subconscious mind that the event visualized actually occurred. This establishes a pathway and a neurological precedent that the body can use and replicate. Proponents of this theory would tell me that the reason why my Centipede visualization sped my clavicle recovery was because during those visualizations I effectively tricked myself and “felt” as though I was healing faster giving my body no alternative but to go ahead and heal faster.
Also at work here is an idea that the physical world or objective reality is the construct of our internal subjective experience. Have you ever noticed that some people have it easy because things always turn out well for them? This idea proposes that it’s the other way around.
The take home here is not the old “Fake it til you make it.” The intent of which statement is to mislead others about your success until you eventually embody that success. Instead, the goal is to “Fake it in a way that some part of you believes it.” The point is to manipulate and mislead yourself so that you will get out of your own way. Still lost? Try this out. To manifest a successful visualization you simply skip the struggle and go straight to the celebration. Here is an example:
Only suckers wait for objective reality. Fire your kids’ soccer instructor. The four step process of scoring a game winning goal in the 2014 World Cup is simple:
1) Remove Your Shirt.
2) Throw Said Shirt Into the Stands.
3) Run In Circles As If Engulfed In Flames.
4) Wait for objective reality to conform to this otherwise irrational behavior.
1-http://www.ncbi.nlm.nih.gov/pubmed/21073100
2-http://www.ncbi.nlm.nih.gov/pubmed/20022993
3-http://www.ncbi.nlm.nih.gov/pubmed/19608100
4-http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2502071/?tool=pmcentrez
5-http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2672052/
6-http://www.ncbi.nlm.nih.gov/pubmed/16368636
7-http://www.ncbi.nlm.nih.gov/pubmed/20508474
8-http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2525972/
Graston Technique: Hard Tools for Soft Tissues
I was in a Graston lecture last weekend when a friend named Dan who is facing knee surgery texted me these probing questions: “What is Graston Technique? Have you had it done? Does it Work? How does it work? How is it different from things like Foam Rolling?” These are pretty good questions and deserve a better answer than my somewhat terse response: “Foam rolling is great, but good luck getting a roll of foam between your femoral condyle and your torn meniscus.” As a favor to you Dan I’ll expand on that answer here.
 |
| Gua-Sha uses Horns, Bones, and Stones |
 |
| The instruments have specialized design features which accommodate the shoulders, elbows, wrists, knees and ankles which make them ideal post-injury and post-surgical tools. |
Lumbar Disc Herniation
It is common for people to wonder if they have a herniated disc in their lower back when they feel pain radiate down the leg. There are several differential diagnoses that must first be ruled out before that conclusion is made. The only way to confirm a herniation diagnosis is with an MRI but a good physical and neurologic assessment is often enough to determine the cause of lower back pain that refers into the leg. If you are wondering if you are suffering from a herniated disc in the lumbar spine and you want to know what your options are, this posting is for you.
- Sudden onset of lower back pain with severe pain down the leg possibly beyond the knee.
- The leg pain may be more severe than the back pain.
- Pain may result from heavy lifting, twisting or repetitive stress trauma.
- The leg pain is described as “electrical”, “sharp” or “shooting.” The pain follows a dermatomal pattern determined by the spinal level of the herniation as pictured below.
- The leg pain is worsened by increases in intra-disc pressure: coughing, sneezing, weight bearing, and positional changes that involve forward flexion of the low back and at the hip.
Additional findings: Dermatomal numbness/ decreased sensation, weakness, decreased reflexes.
- Age 25-45 this is when the nucleus is most hydrated
- male >female 3:2
- Prevalence: 1-3% lower back pain cases
- 95% of lumbar herniations occur at the L4-5, L5-S1 levels
Differential Diagnosis
- Piriformis/sciatica- Sciatica feels like a disc herniation but it is not. Sciatica is when the sciatic nerve is entrapped distally from the spine, typically by a muscle such as the piriformis. This still presents with pain down the back of the leg to the foot and is best treated with chiropractic manipulation of the sacrum and soft tissue work on the piriformis muscle.
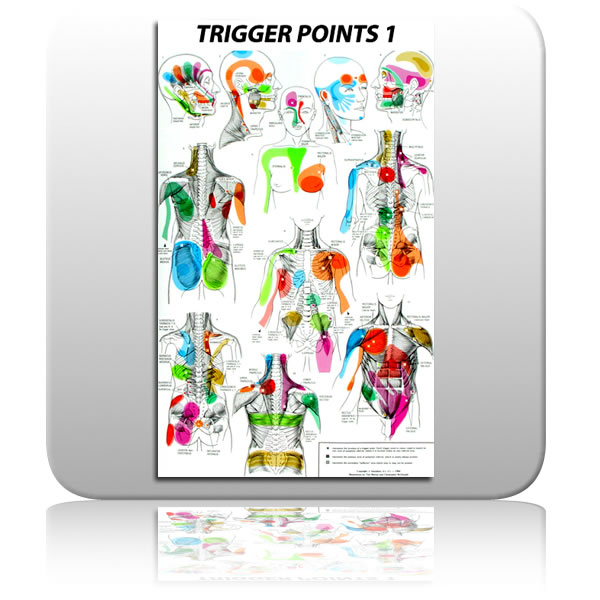
- Myofascial Trigger Point- A trigger point is a small region within a muscle that refers pain distally. They are easily treated with trigger point therapy involving light repeated pressure into the source muscle. The source of this referred pain can be quite a distance from where it manifests as is illustrated in the trigger point map pictured below. Acupuncture also has very effective treatment strategies for trigger points.
- Acute hamstring spasm or strain must also be ruled out as a possible source of sharp pain down the back of the leg.
- Lower Cross Syndrome: A postural shift toward anterior pelvic tilt caused by imbalanced forces across the hips as pictured below. Weak abdominals, a tight lower back, and tight, weak hamstrings and glutes result in excess pressure on the posterior disc fibers.
- Lack of exercise/ poor general health and nutrition. This is why I promote vigorous physical activity with my patient population. I encourage my patients to learn how to safely move very heavy weights and to practice those motions regularly.
Conservative:
Cauda Equina Syndrome presents with saddle parasthesia and urinary retention. It is an emergency situation. Care of all presentations except Cauda Equina should begin with conservative care.
Conservative care of a disc herniation is the non-surgical and drug free route. Except in the case of Cauda Equina Syndrome, this is where all initial care should begin. It involves mobilizing the vertebrae to accomodate the return of the disc material out of the intervertebral foramen. In chiropractic, several techniques are used including Flexion/Extension, The McKenzie Protocol and Chiropractic manipulative therapy. Yes, it is safe to adjust a spine with a disc herniation. It is infact the standard of care. [2] [4] An estimate of the risk of spinal manipulation causing a clinically worsened disc herniation in a patient presenting with lumbar disc herniation is calculated from published data to be less than 1 in 3.7 million. [1] Alternative conservative care modalities include Massage, Acupuncture, and physical therapy.
Surgical:
This is the best option with acute Cauda Equina Syndrome, and is the last option when progressive neurological deficiencies are present during the course of conservative management. That means you are doing the exercises and being adjusted but you continue to digress measurably with loss of muscle strength, tone, and reflexes. Surgery is also the preferred treatment option in cases of sequestration of the disc material into the spinal canal as pictured above. This is a last resort in care because of recent reviews of the literature that reveal even in successful spinal surgeries, the benefits are short-lived and are indistinguishable from conservative outcomes on an 8 year time line. [3] I nearly placed photo of a lumbar surgery in progress here but after the achilles shot last week, I thought that might be too much. For the curious in the group, click here for link to a short youtube video. When going through these videos I found the most interesting part to be the comments left by viewers. They all have had the procedures themselves and they are a solid random sampling of outcomes that reflect a hit and miss level of relief.
Recent MRI studies of asymptomatic populations find that as many as 52% of asymptomatic people have lumbar disc bulges and hernitations! [5] The difference between a benign asymptomatic lesion and a debilitating one is likely your personal biomechanics and how you use your spine day to day. Because of this, the best way to treat a symptomatic disc herniation is to avoid one. An assessment of the biomechanical forces that your lower back is exposed to both statically and with your lifting technique will have you on the right path. If it is too late for that and you already present with symptoms, beginning a course of conservative care now will typically result in 50% improvement in symptoms within the first 3 weeks of initiating care.
Adjust Your Strength: Studies Demonstrate Significant Strength Increases With Spinal Adjustments
I can be a bit of a skeptical person. This makes me difficult to live with but it also makes me a pretty good researcher. It is because of this trait that I shy away from emotion-driven claims on the power of chiropractic to raise the dead and heal all wounds. That being said, a recent review of the literature has opened my eyes and has me a little emotional myself. The research states that my two favorite things- chiropractic and strength gains make each other better. I’m stoked.
I performed a very simple review of literature where I searched the terms “Chiropractic, Strength” in a Pubmed search engine. This is what I found:
I found seven studies that compared full force isometric contraction of muscles including the quadriceps, rotator cuff, cervical extensors and low back extensors before and after chiropractic adjustment of the spine. All seven found increased strength and/or decreased muscle inhibition post adjustment (1,4,6,7,9,10,11). One study showed as much as 66.8% increase in muscle recruitment as tested with surface electromyography (4). These results are compared to placebo groups and control groups. Summary: This is a big deal.
Two of these studies were of particular interest from a sports medicine perspective as they studied the effect of chiropractic adjustment on the vastus medialis oblique of subjects with anterior knee pain (6,7). Both studies found decreased inhibition immediately post adjustment. This is very useful information to anyone trying to regain strength after a knee injury. As any Physical Therapist will tell you, post injury the primary focus of rehabilitation is to activate the VMO which easily inhibits and leads to lifelong strength and stability problems. Take home- if your knee is injured, get your spine adjusted.
The first question I am usually asked when I tell people about the previous studies is “how long after the adjustment do these effects last?” I like this question. It means to me that the patient is trying to plan how fast they’ll have to drive after leaving my office to take full advantage of this phenomena. Two of the above studies attempted to answer this question by performing multiple strength assessments at predetermined intervals following the adjustment. Wang and Meadows 2010 (9) found a measurable increase in the strength of the rotatror cuff muscles for up to ten minutes after the cervical spine was aligned and Grindstaff, Hertel 2009 (10) found acute measurable increases in quadriceps strength of 3% and muscle recruitment of 5% for twenty minutes post adjustment. 3% may not sound like much but if you have a 400 pound back squat, 3% means another twelve hard-earned pounds.
These serial assessments are a difficult way to determine how long the effects last because fatigue obscures maximum efforts. What is also missed by these studies are the accumulative effects of multiple adjustments over the span of a treatment period. These only measure the acute changes after a single adjustment.
I did come across a long-term case study (2) that followed the treatment of an 18 year old patient who had a greatly reduced lumbar curve. The clinician sent the patient to his high school strength coach to test his baseline bench press single repetition max which was 245 pounds. Over the course of a 16 week treatment period which restored his lumbar curve to 31 degrees his bench press max increased by 60 pounds to 305 pounds and he was not bench pressing at all over that entire four month stretch. You would expect his numbers to go down not up. This study supports the premise that a normal lumbar lordosis provides inherent biomechanical stability and strength.
This case study shows the potential for long-term effects but the duration of the study allows for potential confounding factors that can be difficult to control: was he eating and sleeping the same? Was he under the same amounts of stress? It is hard to say. With a larger study with more subjects to compare individual results to you can account for these factors and that sort of a follow-up study is necessary to validate the findings of this case study.
Discussion:
These findings are exciting to most people and everyone who I’ve told about them wants to know: “Why are people stronger after adjustment?” They typically speculate that increased circulation is at work but the idea of increased circulation does not look likely. That wouldn’t explain why adjusting the lower back benefits the strength of muscles up stream in the neck and shoulder girdle (2,3).
It is my opinion that there are two contributing factors to this phenomena:
1) Decreased muscle inhibition, and 2) the effect of stability on strength.
1) Muscle inhibition (MI)-
Would you rather lift a weight with 90 or 99% of your available muscle cells? Decreased muscle inhibition as was demonstrated in the above studies (4,9) means that you have access to a greater percent of your total muscle mass. Inhibited muscle is the percent of your muscle cells that are dormant even during maximum effort. When you decrease MI you are firing on more cylinders. This factor has far reaching potential for long-term strength gains far superior to the acute effects documented in these studies. Accessing and training a greater percent of your muscle mass chronically would have a potentially compounded training effect.
“Why are muscles inhibited in the first place?”
Injury frequently results in muscle inhibition. You could also argue that our modern lifestyle is one that actively fosters MI. How many hours a day do you spend in arch supported shoes and low back supporting chairs?
2) The effect of stability on strength: If the hips are out of alignment and it is potentially dangerous to have the strength to pull 300 pounds over your head your body may have neurologic controls to ensure that you don’t have the muscular strength to over shoot the limitations of your stability. Having a huge overhead press and no lumbar curve is like having a cannon on a canoe.
The old adage “the iron never lies” explains why post adjustment strength is an excellent outcome to measure objectively. The previous studies isolate the effect of an adjustment on a single muscle or group of muscles involved in a motor task but the measurable impact of an adjustment is most likely body wide as is demonstrated by Giggey, Tepe (3) in a 2000 study that exhibited an 8.18 lbs. increase in cervical muscle extensors following a sacroiliac adjustment. This is also evident from the 2009 study by Smith and Dianoff (8) that demonstrated a 9.2% improvement in fine motor skills with a movement time test (rapidly point a pointer at a target on a computer screen) post adjustment compared to control groups.
To better understand the body wide effects of the chiropractic adjustment on the body, a more diverse set of outcome markers that include more motor units would be essential. The above studies only use isometric/static contractions to measure strength changes and it is likely the case that the sort of neurological adaptation facilitated by adjustments is best displayed with explosive movements that involve motor skills and maximal muscle recruitment. Olympic style functional movements such as snatch and clean and jerk would assess both motor skills and muscle strength.
All of your basic body functions may very well benefit from these same adjustments just as skeletal muscle does but it is not as easily studied or measured. The general strength of your immune system for instance may be enhanced post-adjustment but until a “maximum effort contraction” of the immune system is devised we won’t be able to quantify that effect. That will take some clever research design and I will report back when it happens.
1) Hillermann, Gomes, Journal Manipulative Physiological Therapeutics – 2006
2) Morningstar, Grand Blanc, Journal Chiropractic Medicine, Autumn 2003; 2(3):137-41
3) Giggey K, Tepe R., Journal of Chiropractic Medicine 2009 June
4) Keller TS, Colloca CJ, Journal of Manipulative Physiological Therapeutics. 2000, Nov-Dec
5) Jorgen Sandell, Palmgren, Journal of Chiropractic Medicine. 2008 June
6) Suter, McMorland, Herzog, Journal of Manipulative Physiological Therapeutics. 1999. March-April
7) Suter, McMorland, Herzog. Journal of Manipulative Physiological Therapeutics. 2000 Feb
8) Smith, Dianoff, Smith. Journal of Alternative and Complimentary Medicine 2009 March
9) Wang SS., Meadows J. Journal of Manipulative and Physiological Therapeutics. 2010 Feb





