Conditions
Knee Pain and the Kipping Handstand Pushup
If your knee is hurting after last week’s 16.4 workout, don’t be so quick to blame the wall balls. Your kipping handstand pushups may be to blame.
When an athlete does a good job of recruiting the hips in the hspu kip, a violent end range knee extension at lockout is the result. This differs from the crisp knee extension in other movements such as the kettlebell swing because the lower extremity meets no resistance making it an open chain movement with with zero resistance to guide the normal screw-home mechanism of the tibia. The result can be repetitive hyperextension of the knee through the course of say 55 handstand pushups. Add the fact that leaning into the wall to achieve a legal rep further levers the knee into extension, and it should be no surprise that many athletes are limping their way into week 5 of this year’s Open.
Biomechanics of knee extension in hspu-
The likely source of knee pain following a set of kipping handstand pushups is the anterior cruciate ligament. The ACL comes to tension when limiting anterior translation of the tibia at end range flexion. In hyperextension, the ACL is vulnerable to impingement by the intercondylar notch roof of the femur. See article HERE.
The Take Home- Explosive knee extension in a kipping hspu is different than in other movements. The legs are flailing into the sky without any resistance to prevent hyperextension. The result is like the ACL getting slammed in a door.
Presentation-
The result of this repetitive ACL impingement is inflammation within the joint space and pain at end range flexion. The inflamed joint feels unstable, clicks and pops but should not lock up or give way. Getting into the bottom of a squat is very difficult in the week that follows this injury as the joint is swollen on the posterior side and the aggravated ACL is at tension at end range flexion of the knee.
Preventative measures-
Knee sleeves and Rock Tape
- Neoprene knee sleeves
- Hamstring Rock Tape
- Adds some tactile awareness of knee end-range
Joint Prep-
- Coactivation Exercises- Russian Swing/ Power Swing
- Focus on coactivation of glutes with quads to avoid end range extension.
- Hamstring prep- Death March/ Kang Squat
Technique-
- Coactivate glutes, hamstrings, and quads during knee extension.
- Stay on the wall. Striking the heel into the wall at the top of the motion increases hyperextension forces. If possible, glide the heels up the wall as the knee approaches lock out.
- Closer hand placement-
- The further the hands are from the wall, the greater the knee is leveraged into hyperextension at lockout.
Recovery-
It is unlikely that serious mechanical damage has taken place. If you have apprehension or are experiencing locking up or giving way of the joint, have it assessed by your local knee specialist. Otherwise you are dealing with painful inflammation of the ACL.
Inflammatory measures- 4-7 days
Heat / Ice contrast therapy. 6/1 ratio
Normatec vasopneumatic compression
- 20 minute sessions level 8
- 3x/day on empty stomach
Voodoo Floss
- The poor man’s normatec
Pray that there are not pistol squats in 16.5.
Hamstring Strain: Rehab For Rapid Recovery
How do you know if you pulled/ strained/ or tore your hammy? You’ll know. A good sign that you are about to tear your hammy is that your age to strength ratio is out of balance and you are about to play flag football.
Prognosis:
A grade one strain is the most common and is what is usually referred to as a “pulled hammy.” These should still be taken seriously in the first 3-5 days as it doesn’t take much to turn a grade one strain into a grade two, or a grade two strain into a grade three. As a general rule, grade one hamstring strains should be rested from competitive sporting activity for about 3 weeks and grade two injuries for about 4 to 6 weeks. In the case of a complete rupture, the muscle will have to be repaired surgically and the rehabilitation afterwards will take about 3 months.
If you know any athletes you know that these general rules are almost impossible to enforce when there is a game to be played. For that reason let’s explore some techniques to accelerate this lengthy and tedious healing curve.
1) Avoid the Injury:
- Build up to full speed over time when preparing for a max effort sprint particularly when recovering from a hamstring pull. You’ll need 10 minutes of general warm-up before getting serious. An example of escelating intensity post warm-up could look like: 100m @ about 85%, 200m@ 85%, 300m @90% before going 100% on subsequent 400m, 300m 200m and 100m. This scheme would have been a good idea for me a week ago.
2) Rehab the Injury:
- Control inflammation in the first 3-5 days–
- RICE (Rest, Ice, Compression, Elevation) I iced 5-7x/day for 10-20 minute spells
- Anti-Inflammatories- I do not recommend NSAIDs, but I have had success with the topical anti-inflammatory Traumeel. It is better than tiger balm. I know this to be blasphemous among many of my mentholated friends but traumeel is a blend of topical anti-inflammatory herbs supported by research and found to be equally effective at combating inflammation as NSAIDs but with a different mechanism without NSAID’s well documented side effects.
- Avoid inflammatory foods by going paleo for the initial 3-5 days at a minimum.
- High-end your fish oil intake. I went to 4 tbs./day for the first 5 days.
- Reduce muscle spasm– Muscle spasm is a common and painful symptom of a hamstring injury. Because of the trauma to the muscle, signals of contraction are confused, and the muscle may be stimulated.
- Keep the muscle lengthened but not stretched.
- Avoid the seated position as much as possible.
- General soft tissue work can help with both the inflammation and the spasm of an acute strain. We’re not talking deep tissue massage here. I used Graston on mine on days 2-5 by day six I was feeling pretty good. Rather than breaking up adhesions, the goal was to facilitate healing by combing the broken edges back together.
- Other useful techniques are foam rolling and pin and stretch.
- Increase growth hormone and healing factors to your leg by continuing to train vigorously– The hamstring is off limits for a while so hit everything else like it owes you money. This is your chance to break away from those righteous functional movements and indulge in a Jersey Shore-esque upper body jackage fest. Baby oil, while lacking any medicinal or anti-inflammatory properties, is often liberally applied to the arms during and after these workouts. Go ahead and hit those bench presses, those bicep curls and don’t forget the shrugs. For cardio, you can remove all of the sleeves from your t-shirts for time. Enjoy yourself. You’ve popped your hamstring and you deserve it.
 |
| Fist Pump’n Like a Champ. |
What is an Exertional Headache?
The pain of a primary exertion headache is the result of compromised biomechanics in the neck leading to a spasm of the suboccipital muscles that attach the base of your skull to your neck. This results in increased blood pressure in the vessels in the brain and causes a benign but exquisitely intense wave of throbbing pain that can last between 5 minutes and 24 hours.
There are two classes of exertion headaches: Primary and Secondary.
1) Primary Exertion Headaches are the direct result of high exertion and simple biomechanical factors without an underlying pathology. Approximately 3% of the population suffers from benign primary exertional headaches. (Neurology. 1996;46:1520-1524)
2) Secondary Exertion Headaches are exertion headaches that crop up because of an underlying lesion such as a brain tumor or brain hemorrhage. While the vast majority of exertion headaches are of the primary benign variety, sufferers of exertion headaches have an increased rate of intracranial lesions when compared to the general population according to numerous published studies.
If you are having exertion headaches, you would be well advised to have your medical doctor give you a physical to rule out signs of the worst case scenario. Ideally, this would be a physician with a sports medicine background so as to avoid the irritating questions of “why do you lift heavy things?” “Don’t you know that squatting below parallel is bad for your knees?” or “who told you that is how people procreate?”
How to Address Primary Exertional Headaches
When someone presents in my office with an exertional headache I address the biomechanics of the neck with cervical traction, Graston Technique for deep soft tissue work, and a chiropractic adjustment called an occiput lift. Due largely in part to the Crossfit Games Open wod #4, I have had many opportunities to work on exertional headaches lately and this combination gets results.
K-Starr has some handy self care techniques that will keep your symptoms in check long enough to get an appointment with someone who can do some corrective work for you.
Is it safe to continue training with exertional headaches?
To get back to normal training, it is typically the case that you have to lower your intensity levels and go 1-2 weeks without inducing the headache before you can return to normal levels of pain free exertion.
Primary exertional headaches are benign. After getting confirmation from your MD that there’s no underlying cause, it is safe to train with or through the pain. It is however not always possible to continue to train as it feels as though you have been punched in the brain and Trent Reznor has built a nest behind your eyes.
Graston Technique: Hard Tools for Soft Tissues
I was in a Graston lecture last weekend when a friend named Dan who is facing knee surgery texted me these probing questions: “What is Graston Technique? Have you had it done? Does it Work? How does it work? How is it different from things like Foam Rolling?” These are pretty good questions and deserve a better answer than my somewhat terse response: “Foam rolling is great, but good luck getting a roll of foam between your femoral condyle and your torn meniscus.” As a favor to you Dan I’ll expand on that answer here.
 |
| Gua-Sha uses Horns, Bones, and Stones |
 |
| The instruments have specialized design features which accommodate the shoulders, elbows, wrists, knees and ankles which make them ideal post-injury and post-surgical tools. |
Lumbar Disc Herniation
It is common for people to wonder if they have a herniated disc in their lower back when they feel pain radiate down the leg. There are several differential diagnoses that must first be ruled out before that conclusion is made. The only way to confirm a herniation diagnosis is with an MRI but a good physical and neurologic assessment is often enough to determine the cause of lower back pain that refers into the leg. If you are wondering if you are suffering from a herniated disc in the lumbar spine and you want to know what your options are, this posting is for you.
- Sudden onset of lower back pain with severe pain down the leg possibly beyond the knee.
- The leg pain may be more severe than the back pain.
- Pain may result from heavy lifting, twisting or repetitive stress trauma.
- The leg pain is described as “electrical”, “sharp” or “shooting.” The pain follows a dermatomal pattern determined by the spinal level of the herniation as pictured below.
- The leg pain is worsened by increases in intra-disc pressure: coughing, sneezing, weight bearing, and positional changes that involve forward flexion of the low back and at the hip.
Additional findings: Dermatomal numbness/ decreased sensation, weakness, decreased reflexes.
- Age 25-45 this is when the nucleus is most hydrated
- male >female 3:2
- Prevalence: 1-3% lower back pain cases
- 95% of lumbar herniations occur at the L4-5, L5-S1 levels
Differential Diagnosis
- Piriformis/sciatica- Sciatica feels like a disc herniation but it is not. Sciatica is when the sciatic nerve is entrapped distally from the spine, typically by a muscle such as the piriformis. This still presents with pain down the back of the leg to the foot and is best treated with chiropractic manipulation of the sacrum and soft tissue work on the piriformis muscle.
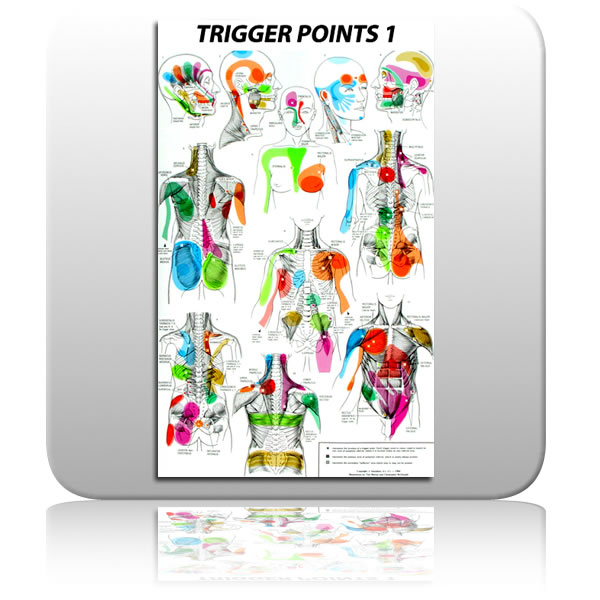
- Myofascial Trigger Point- A trigger point is a small region within a muscle that refers pain distally. They are easily treated with trigger point therapy involving light repeated pressure into the source muscle. The source of this referred pain can be quite a distance from where it manifests as is illustrated in the trigger point map pictured below. Acupuncture also has very effective treatment strategies for trigger points.
- Acute hamstring spasm or strain must also be ruled out as a possible source of sharp pain down the back of the leg.
- Lower Cross Syndrome: A postural shift toward anterior pelvic tilt caused by imbalanced forces across the hips as pictured below. Weak abdominals, a tight lower back, and tight, weak hamstrings and glutes result in excess pressure on the posterior disc fibers.
- Lack of exercise/ poor general health and nutrition. This is why I promote vigorous physical activity with my patient population. I encourage my patients to learn how to safely move very heavy weights and to practice those motions regularly.
Conservative:
Cauda Equina Syndrome presents with saddle parasthesia and urinary retention. It is an emergency situation. Care of all presentations except Cauda Equina should begin with conservative care.
Conservative care of a disc herniation is the non-surgical and drug free route. Except in the case of Cauda Equina Syndrome, this is where all initial care should begin. It involves mobilizing the vertebrae to accomodate the return of the disc material out of the intervertebral foramen. In chiropractic, several techniques are used including Flexion/Extension, The McKenzie Protocol and Chiropractic manipulative therapy. Yes, it is safe to adjust a spine with a disc herniation. It is infact the standard of care. [2] [4] An estimate of the risk of spinal manipulation causing a clinically worsened disc herniation in a patient presenting with lumbar disc herniation is calculated from published data to be less than 1 in 3.7 million. [1] Alternative conservative care modalities include Massage, Acupuncture, and physical therapy.
Surgical:
This is the best option with acute Cauda Equina Syndrome, and is the last option when progressive neurological deficiencies are present during the course of conservative management. That means you are doing the exercises and being adjusted but you continue to digress measurably with loss of muscle strength, tone, and reflexes. Surgery is also the preferred treatment option in cases of sequestration of the disc material into the spinal canal as pictured above. This is a last resort in care because of recent reviews of the literature that reveal even in successful spinal surgeries, the benefits are short-lived and are indistinguishable from conservative outcomes on an 8 year time line. [3] I nearly placed photo of a lumbar surgery in progress here but after the achilles shot last week, I thought that might be too much. For the curious in the group, click here for link to a short youtube video. When going through these videos I found the most interesting part to be the comments left by viewers. They all have had the procedures themselves and they are a solid random sampling of outcomes that reflect a hit and miss level of relief.
Recent MRI studies of asymptomatic populations find that as many as 52% of asymptomatic people have lumbar disc bulges and hernitations! [5] The difference between a benign asymptomatic lesion and a debilitating one is likely your personal biomechanics and how you use your spine day to day. Because of this, the best way to treat a symptomatic disc herniation is to avoid one. An assessment of the biomechanical forces that your lower back is exposed to both statically and with your lifting technique will have you on the right path. If it is too late for that and you already present with symptoms, beginning a course of conservative care now will typically result in 50% improvement in symptoms within the first 3 weeks of initiating care.
Achilles Tendon Injury
Injuries to this part of the body go by many different names depending on location and severity of injury: Achilles rupture, achilles tendinitis, achilles tendinosis, tennis leg, gastroc strain, soleus strain, the list goes on but I will refer to the rupture of a lower leg tissue generally as an achilles strain from here on out. The purpose of this post is to help the reader avoid ever having this injury by recognizing risk factors and developing skills that neutralize those risks.
The achilles tendon is the largest and strongest tendon in the body. It can sustain a tensile load of 1 ton. That is the weight of a VW beetle. Despite it’s inherent strength, it remains the second most frequently torn tendon in the human body. The achilles is as substantial as it is because it is made to withstand the dynamic stress of an eccentric load. What that means is that when you jump and land on your toes, the gastrocnemius contracts to slow your heel from hitting the ground at the same time that it lengthens to accommodate dorsiflexion at the ankle. That makes the achilles tendon a rope in a powerful tug of war. When you gain strenth, weight, or increase work load rapidly, you run the risk of out pacing the relatively avascular tendon’s ability to adapt resulting in pulling it apart with your own body’s forces.
Because of the inherent strength of this structure, it is unlikely for it to tear or rupture when it is healthy. It is far more common for a previously inflamed gastroc-achillis complex to give way to a major tear. This is a peculiar tissue that runs when it is torn, much like a piece of paper with a small tear in it- pull on both ends and you’ll soon have two pieces of paper. Athletes are used to performing through discomfort and pain and rarely take the necessary steps required to avoid an impending tear. Most of the successful athletes that I know don’t “listen to their bodies.” They have another chain of command where their bodies do as they are told. That being said, have a look at the wrecked tendon below. This is what was left of my older brother’s achilles after he blew it out in a basketball game. He played through the pain. He went to the gym the next day! He didn’t get in to have it looked at for 3 days. I love him, but he’s a big dumb animal. Don’t be a big dumb animal.
Know when you are vulnerable:
There are 3 major ways that you may be vulnerable to an achilles injury right now.
1) Demographic:
Are you an athlete between the age of 25 and 40?
Have you recently gained weight or increased your strength?
2) Achilles Abuse
Do you like to train cold? Take off from a stop to a sprint? Do you do workouts with rapid repetitive jumps? Do you frequently run on the road? Are you experimenting with barefoot running?
3) Previous Injury
Are you sore and tight above your heel when you first wake up in the morning? Does it wear off as the day goes on?
Have you noticed any swelling making one calf muscle appear larger than the other? Remember it doesn’t have to be painful.
Have you noticed a “twang” in that area. The day after a REALLY long run I felt the sensation of guitar strings being strummed in my achilles followed by them being cut one by one. I iced it and steered clear of dynamic training for a week.
This injury can still be avoided even if you meet several of the at risk criteria above:
Be Proactive:
Listen to your body- I know. You don’t want to but when your body speaks from your lower leg you listen. When your lower leg hurts even a little, ice it and give it space.
Warm the area. I don’t mean “warm up.” Waving your arms and crunching your core won’t warm your achilles tendons. Use the muscle before you stress it and for God’s sake don’t warm up with double jumps or you’re asking for trouble.
Make gradual progressions- The 10% rule is a conservative way of extending your distances by 10% per outing.
Train on diverse surfaces- Consistently running forward on pavement will overwork the mid line structures of your lower leg.
If you are experimenting with the idea of bare foot running, do it step by step- Losing the heel you’ve had you’re entire adult life places an additional 1/2 inch stress on your achilles/gastrosoleus junction.
Stretch the gastroc statically post work out and throughout the week- This can be done with simple moves such as down dog but I like this wall stretch posted to MWOD last month. The guy (K Starr) yammers on for 3 minutes before he gets down to it, but there is a quality mobility in the end:
Keep in mind that the gastroc is part of a larger fascial plane that runs from the bottom of your foot to the origin of your hamstring at your ischial tuberosity. Maintain global range of motion all the way to the toe by working a ball into the base of the foot while you are at your desk.
Summary:
If you injure your lower leg it is typically all or nothing:
All- you feel like you’ve been kicked, hit, or shot in the back of the calf. You will probably even turn around to see who did it. It may hurt a lot as in a 1st or 2nd degree tear, or it may only hurt a little as with a total rupture which can be less painful due to the nerve damage. Either way, it will probably swell and a palpable lesion may be present. Tape your ankle into plantar flexion and get to a sports medicine doc as soon as possible. Do Not Stretch It.
Nothing- This is the small lesion or inflammation that later leads to “All” as described above. With a chronic presentation of lasting discomfort in the lower leg, fascial adhesions are likely built up between the muscle and the fascia. The soft tissue modalities of ART and Graston Technique (tools pictured below) are the methods of choice for releasing those adhesions before they cause larger problems.
 |
With an acute onset PRICE is the rule here: Protect, Rest, Ice, Compression, Elevate. Remember that the P in protect may require you to Protect your lower leg from your ego and whatever achilles busting plans you had for it when you woke up this morning.